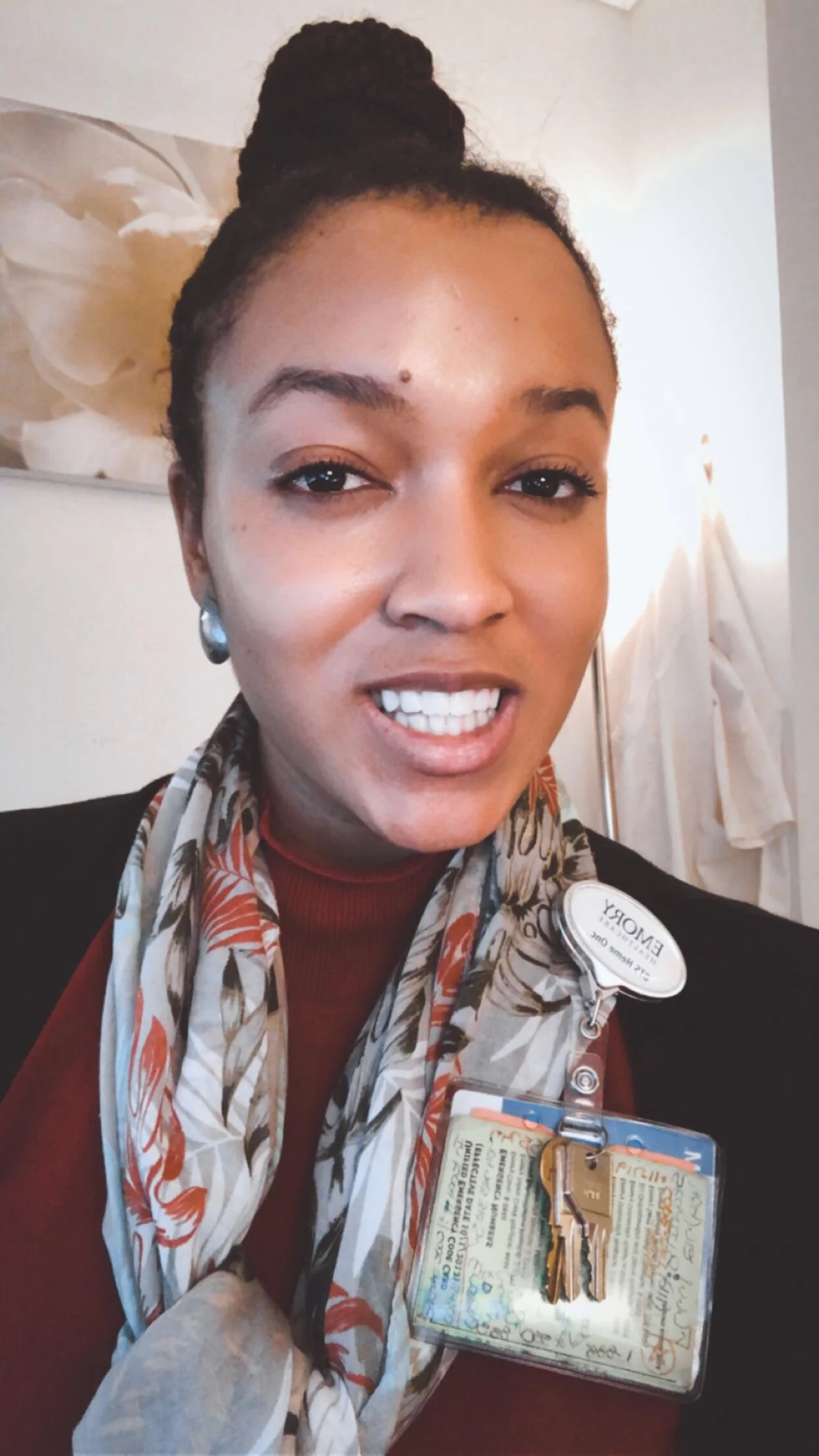
Denise Asafu-Adjei, Resident Physician - Urology
Hi, Denise! What do you do, and given how specialized it is, how would you describe it to someone unfamiliar with that space?
I am a resident physician, which means that I have finished medical school. My sub-specialization is in the area of urology which has a focus in the surgical management of the urinary system, including the kidney, bladder, prostate, and the penis.
Can you describe your educational path?
I was born and raised in the Bronx, and attended probably one of the country’s most famous magnet schools, the Bronx High School of Science. I then attended Carnegie Mellon University, majoring in biological sciences. At that point, I knew I was going down the medical path. I’ve always been interested in the science field, so in college medicine felt like the best match. I went to the University of Michigan for medical school, and took a year off to do a master’s of public health at Harvard’s Chan School of Public Health with a focus on healthcare management. Currently, I’m a chief resident in my last year of residency in urology at Columbia University Medical Center. So, I took a fairly straightforward path for a physician. The one difference is my MPH, which at the time wasn’t as common, but the trend is on an upswing now.
What attracted you to urology, specifically?
This is always an interesting question. When I went to medical school, I didn’t want to do surgery. As I started doing clinical rotations, I became drawn to surgery but thought I would do primary care or pediatrics. When I decided on surgery, I was getting ready to start my MPH at Harvard. Part of my spirit was not sold on general surgery. I knew that I liked working with my hands and liked the immediate gratification after completing a procedure for a patient. What really shifted my attitude on surgery was the passing of my uncle who had metastatic kidney cancer. When he was getting evaluated in Ghana, I was trying to read more about the field because I had no idea what type of physician took care of people with kidney cancer. To help my family determine who my uncle needed to speak with, I read so much information on the urology field, and I came away feeling like that specialization would satisfy my own surgical interests. I also knew that there was some versatility to change my focus if that’s what I wanted, which also drew me to the specialization. It’s also an area where you can still have a solid work/life balance.
Why is it a better work/life balance for this particular area?
Urology is a subspecialty within surgery, and within surgery there are so many choices for what you can do based on how frequently you want to be in the operating room. If you want to operate all day, there are subspecialties where you can do that. As I have gotten older and developed more ownership over my future, I know what I want, and I know what I don’t want. Being happy, having the opportunity to have a family — these things are what really matter to me. Urology offered the ability to have that kind of balance. Soon, I’ll be starting at UCLA for a fellowship in sex medicine and male infertility, which is a fairly heavy clinical-based practice with some OR time, but not overwhelmingly so.
Who has been a major influence for you?
Not to sound cliche, but my parents. They’re both very persevering. We may have had no heat on growing up but they always made sure our school fees were paid for. My family really appreciates education, and I think my parents could have both done a lot more outside of what they did when they came here forty years ago as immigrants. But they always put us at the forefront. They inspire me every day with the deep love they show me and my siblings.
In the little time off that you have, what do you like to do?
I enjoy going to the theatre and to the movies. I love live performances. Spending time with my family is always a huge plus. I also really like physical activities to keep myself in shape. Me and my partner picked up golf a couple of months ago. I appreciate trying things I never thought I’d do. I also really like politics and policy, and understanding how systems work. And traveling — love, love, love traveling.
Have you had any especially challenging experiences?
During medical school, you have to take the United States Medical Licensing Examination, or what is more commonly called “the STEPs.” It includes all of the things you have to do to apply for board certification when you apply for residency. We don’t have formal grades. It goes by how you’re doing in the class. It’s a required exam, and in the first part of the series, I had studied probably the most intensely I have ever studied in my life. I would start at 6 a.m. and go until late. I was studying so much but I didn’t do as well on the exam as I had hoped. When you’re coming from a place when you’ve always been on top and nothing has been hard, it’s challenging. From the standpoint of “lessons learned” it was actually really good to see that I need to take care of myself. I had been practicing this physical martyrdom that just wasn’t sustainable. I needed to be happier with myself, and that attitude transferred into decisions I would make for myself later on.
Can you share a bit on your UCLA program you’ll be beginning soon?
I start my program in July 2020 and, as I said, I will sub-specialize in male sex and infertility. My ultimate goal is to shift the paradigm of policies around reproductive health. There’s lots of red tape around IVF [in-vitro fertilization] and sponsors and donors. I’ve always felt that minorities often have not been able to tap into IVF because of the associated costs, so I’m hoping to create better access.
That’s incredible. And so, finally, what are you excited about for the future?
In so many ways, I have felt genuinely blessed. In the short term, I’m excited for more travel. Recently I traveled to Greece, and I went to Ghana for New Year's. I try to get away when I can, because I deeply feel that you have to recalibrate in order to continue on.
On a larger level, I think I’m excited about the tide of women of color that have begun to emerge and to ascend in every realm of society. I’m excited about the true diversity of this country being reflected in everything we do, and I think that value—diversity—is being recognized and respected more. I’m obviously biased because I’m a woman and I’m black, but I think it’s exciting.
I also get excited about my speciality. Being able to help people have children and an improved quality of life through healthy sex lives. Happy, healthy people create happy, healthy societies, and any way I can contribute to that is great.
Please share this post with a friend, and follow us at @BlackWomenWorkIG!