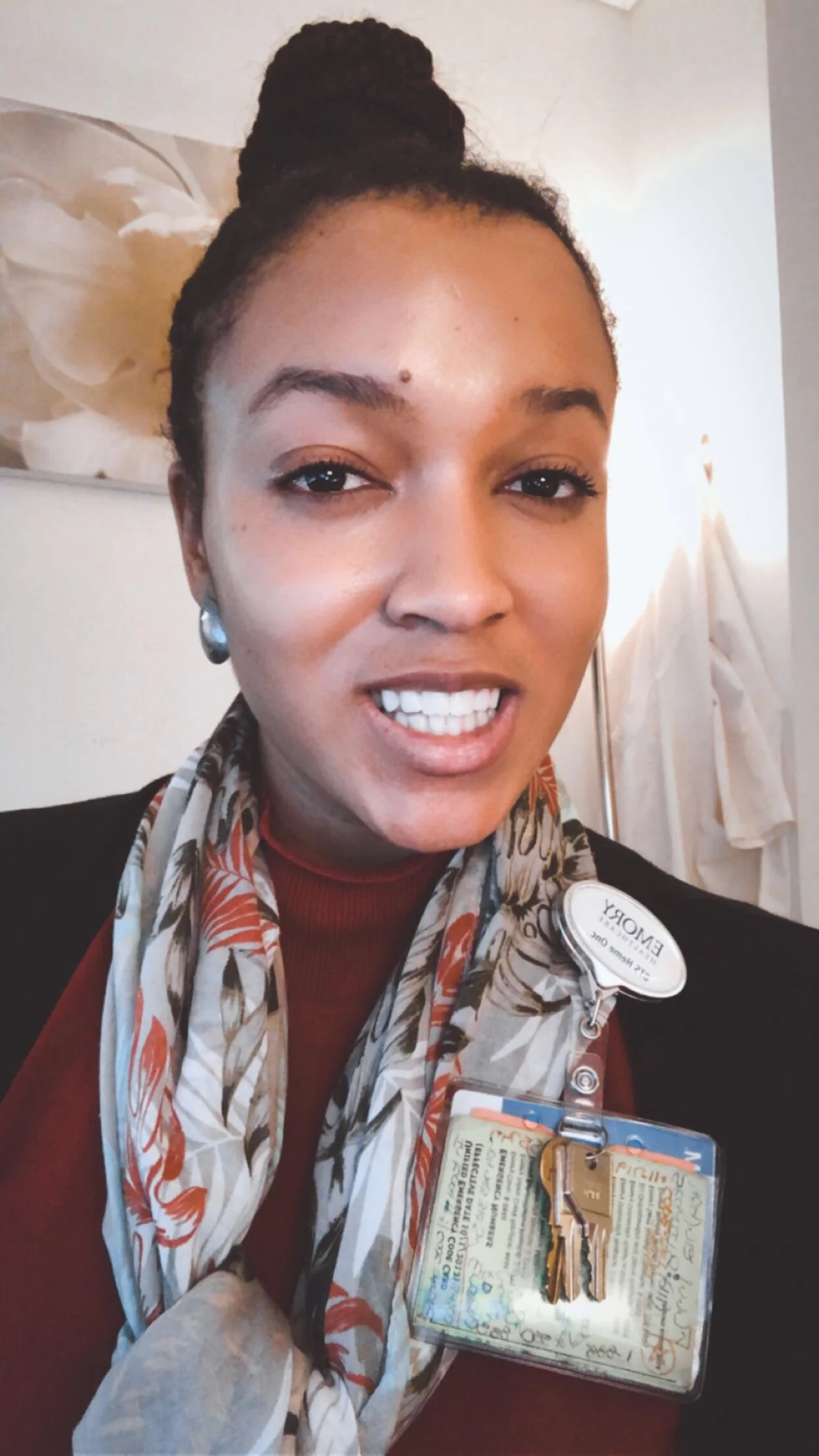
Alysson Perrin, Advanced Practice Registered Nurse & Oncology Nurse Practitioner and Clinical Nurse Specialist
Hi, Alysson! What do you do and how would you describe it to someone unfamiliar with your profession?
I’m an advanced practice registered nurse (APRN). There are four types of APRNs, and I’m licensed to practice in two of the roles, which is rare — a nurse practitioner (NP) and as a clinical nurse specialist (CNS). So when you think of a nurse, you probably think of a registered nurse (RN). RN’s typically work in an inpatient hospital setting caring for the needs of patients who have to stay based on their medical condition. RNs also work in an outpatient clinic or office setting. In both settings, RN’s implement the treatment plan as typically outlined by the physician.
As an APRN, I am an RN with advanced education, training and licensure to assess, diagnose, order tests, and prescribe medications to manage patient medical problems. Depending on the medical needs of the patient, APRN’s can work independently as a medical provider or we can work with a physician to assist in managing their patient population.
So what kind of setting are you in right now?
I work in an inpatient hospital setting with adult oncology patients.
What attracted you to nursing?
I was always taught that I needed to pick a major that would provide a career that would quickly allow me to pay my own bills. (laughs) But also, I truly enjoy helping people. In high school, I figured out that I wanted to be either a teacher or a nurse. I volunteered at a hospital when I was in high school on summer breaks, but I mostly only filed papers in the medical record room so it wasn’t a good experience. So I thought I would go with teaching.
In undergrad, I signed up for all the School of Education prerequisites and landed a teaching internship the summer after my freshman year called Summer Bridge. During the internship, college students teach inner-city students for a summer in preparation for the upcoming school year. I taught 7th and 8th grade African and Asian history in Atlanta. While I love kids they can be a handful to say the least. (laughs) And their parents can be quite a handful, too. I realized pretty quickly that teaching was not for me.
I continued volunteering at a hospital in college, and that second time around, I actually had interaction with patients which was such a rewarding experience. In re-considering what other careers would involve helping people and securing a job after graduation, I landed back on nursing.
What are the highs and lows of nursing for you?
The highs are that I really get to know my patients. I spend time with them through the trajectory of their diagnosis, during treatment, and at the end whether that means remission or end-of-life care. You get to know their families and close friends as well who are a part of their support team. I appreciate that interaction. It’s very fulfilling for me. In other areas of nursing, you don’t really get the opportunity to know patients as well because they come and go, you may never see them again. But in oncology, it is not like that. It’s really an honor to be able to take care of my patients. I also have had several family members who have had cancer so I feel as if I am giving back.
The lows are that it can be really sad. Sometimes there is nothing you can do as a medical provider when an outcome for the patient isn’t ideal, or there’s a loss of life. That’s part of working in healthcare.
That sounds challenging. What would you say are some of the technical challenges you’ve experienced?
In one of my APRN roles as a CNS, I am a part of the inpatient nursing leadership team for the oncology service line, so my focus is supporting nursing staff at the leadership level to provide high quality care. One challenge is getting nurses at the bedside to document patient care in a way that is needed for compliance. Another challenge is coming up with new ways to meet our quality metric goals. An example would be preventing central line bloodstream infections from occurring.
What do you do for yourself, and for self care? How do you pour back into yourself given how much you’re doing for others?
I love going out to eat and trying new restaurants. It brings me joy. (laughs) I love traveling and exploring different cities. My last big trip was to Lagos, Nigeria and I had a great time. I also enjoy having quiet time to myself to just reflect and journal. If I’m stressed, I write it down. That’s almost all of the entries because I only really journal when I am stressed. So those are the things that are helpful to me.
I know you’re in Atlanta which is a city with a large black population, but I’d imagine there are still unique aspects to your experience given the profession you’re in. What is it like as a black woman in a leadership role at a hospital?
It’s funny because, yes, I work in Atlanta and I used to work in Houston. Both cities have large black professional populations. In my experience, healthcare leadership is not as diverse, with an exception being leadership teams at hospitals that serve a majority black population.
I have also noticed it’s not just a lack of diversity, but often a considerable generation gap. Many healthcare leaders are closer to the retirement end of things and have been working for a long time. If the leadership role is not nursing related, it is also often male-dominated. For example, executive healthcare leadership teams may only have one woman at the table who is often the chief nursing officer. My concern is that until this generation of leaders retire there won’t be opportunities for a more diverse demographic of health care leaders. In the meantime, I’m frequently find myself trying to fit in professionally with people who don’t look like, who are of the opposite sex, and who aren’t my age.
Honestly, it can be draining sometimes. It takes energy to fit in spaces that were not originally created for me. But it’s important for me to be there to help these spaces diversify. I’m grateful to have a seat at the table and continue to hopefully move up in healthcare leadership. Hopefully I will have an opportunity to bring individuals from diverse backgrounds into these roles. Because we’re out here! (laughs)
Do you think that there are industry reasons for why there are not more black APRNs?
One possible reason is lack of accessibility. If you are working full time it is hard to go back to school to obtain your MSN to become an APRN. Also in nursing school you have to complete clinical rotations which is a part of your training where you learn in a patient care setting outside of your classroom time which also competes with other life priorities. I do think the trend may be reversing, because a lot of nursing programs have more flexibility. So you can go back to school and complete some classes partially online, as well as in person. Some hospitals are doing reimbursements for going back to school as well as repaying loans. Becoming an APRN is more accessible and more minorities, I hope, will take advantage. There are more MSN programs that are accommodating to different lifestyles.
Can you think back to a big learning moment that really made you feel like you’d really found your footing?
Yes, my first job as a nurse practitioner. I started and immediately was like, “What did they just teach us in school?” (laughs) It was such a big change from clinical rotations to actually caring for patients independently and making medical decisions for them. I learned that I did actually have all the tools I needed to succeed but that first six months is tough. It’s a role change, and you’re used to working as an RN and—to an extent—having someone telling you what you need to do. Now you’re the one helping to develop a treatment plan for the patient or an RN to follow.
What advice would you give to young women seeking to get into this space?
I suggest doing your homework. There are lots of different APRN roles. A lot of people just want to get off the floor or out of the clinic so they think, “Oh, I’ll go be an NP.” There’s not much thought to all the types of programs available, or the variety of settings you could work in as an RN. So people are choosing programs where there are so many people going into that specialty you may have trouble getting a job post graduation. I would recommend considering what your priorities are and the work environment you want, and do your research. Take your time to figure out what is best for you.
When you think about your future, what makes you excited?
I think what makes me excited about my future is the impact I can have at different levels. I think I’ve realized no matter what role I have or what level of nursing I am at, I can make an impact and bring a different perspective and a different set of experiences to the table. Most people don’t do multiple APRN roles. They usually only have the credentials to do one of the four. I think what makes me excited is knowing I have an advantage because I understand both the behind the scenes leadership side of healthcare, and also the direct patient care side of healthcare. That sets me apart and creates a lot of unique opportunities for me to explore.
Please share this post with a friend, and follow us at @BlackWomenWorkIG!